Your #1 PEO News Source
Latest Posts
- ACA Taxes
- About PEO
- Brokers
- Bureau Rate Change
- Business Insurance
- COVID Relief
- COVID-19
- Cannabis / Marijuana D...
- Captives
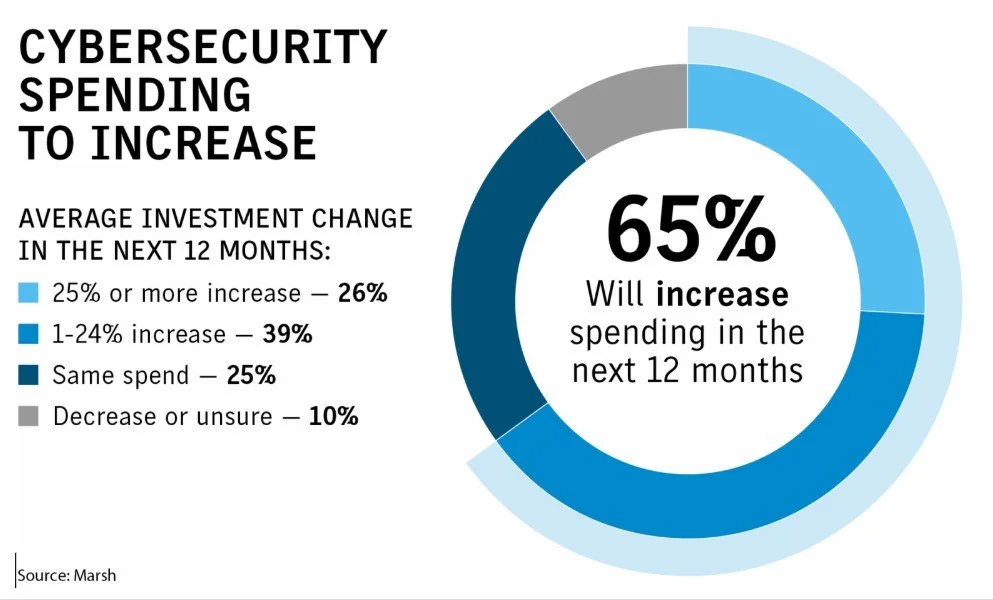
- Cyber Security and Lia...
- Data, Analytics and Ma...
- Department of Labor
- Employment Practices L...
- Events
- Health Insurance
- Industry News
- Innovation and Technology
- Insurance
- Legislation
- Mergers and Acquisitions
- News Round-Up
- OSHA
- Occupational Accident ...
- PEO Industry News and ...
- Phishing
- Specialty Casualty Ins...
- Sponsored Content
- Underwriting
- Video Interviews
- Workers Compensation
- Workplace News and Tips
- ftc
- napeo